July is sarcoma awareness month so I’ve invited others affected by sarcoma to guest blog throughout the month. Today’s blog comes from Suzanne Burkhart, wife to a sarcoma angel, Jim Burkhart.
When my husband Jim told me he had Sarcoma, I looked at him and said “Are you sure the doctor didn’t say ‘Carcinoma’”? “No, the doctor said Spindle Cell Sarcoma”. Sarcoma, what was that word?
Our journey began before the “Sarcoma” word. In January of 2011, my husband Jim was watching one of many bowl games when he felt a lump on the back of his leg. He pushed on it and immediately pain shot down to his foot. He kept that information to himself. A few weeks later, I walked into our bedroom to see Jim stretching out his leg. I asked what he was doing and he replied “I think I tore a muscle, so just stretching my leg”. I suggested physical therapy.
The physical therapist said he would not touch Jim until he had an MRI. That MRI led him to surgery for a biopsy. Right before Easter of 2011 Jim was told the dreaded news – Spindle Cell Sarcoma and an appointment was scheduled for the Monday after Easter at the University of Iowa.
We met with Dr. Joseph Buckwalter and he explained more about sarcoma, but your mind is a whirl and you don’t fully comprehend. Jim was scheduled for surgery that Friday in hopes to clean up the tumor, to get a full understanding of what we were dealing with. Friday’s surgery came and after surgery, Dr. Buckwalter told me that in order to save Jim’s life, he would have to amputate the left leg. I cried….whatever else was said I don’t remember other than those words “we are going to have to amputate”.
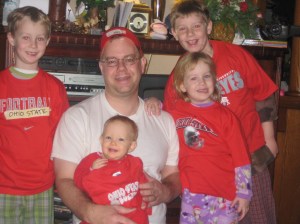
We went home to tell our children. Sam was 9, Henry 8, Eleanor 5 and Charlotte had just turned two. How do you find the words to tell your kids that their world was going to change, that their dad was going to look different. Our family cried, the boys begged for it to not happen, that they would be better behaved, we prayed. We went back to Dr. Buckwalter to discuss the amputation.
Due to scheduling conflicts (ours because we wanted to wait until after our son’s First Communion) we met with Dr. Ben Miller. We really felt at ease with Dr. Miller. Dr. Buckwalter was a very good doctor, but at the time, I was very angry with Dr. Buckwalter for the news he had delivered. Surgery was scheduled for May 20- Jim and my 11th wedding anniversary. For me, what better day, since I promised Jim, in sickness and in health.
I think around this time we were introduced to Dr. Milhem. We were told to call him Mo. He didn’t sugar coat, he didn’t make promises but he got down to business, his business, of understanding and treating Sarcoma. The first form of business was to find out that we were dealing with Synovial Sarcoma. Visit after visit, we either came out of Mo’s office with a sense of relief in knowing that the cancer was behaving itself or with a new plan of chemo or clinical trial. Never once did Mo ever fill us with false hope if he didn’t have an answer as to why the Sarcoma was behaving a certain way. He would give us the “I need to talk this over with my colleagues to see if other doctors had any type if sarcomas acting this way. Email me tomorrow and I will have an answer.”
This is how it is with Mo. Our lives were up and down and he was the steady in our tumultuous waters. We went for a second opinion in New York and came back to Mo with our findings. We went to NIH (National Institutes of Health) with Mo’s blessing for Jim to be in yet another clinical trial. We always pushed Mo and he pushed further and harder for Jim.
In March of this year, Jim had a gall bladder attack. With everything he had going on, a gall bladder attack seemed minor. We had our local doctors make contact with Iowa on how to treat. A week off of treatment and Jim had his gall bladder removed. Another week off of treatment and Jim was chomping at the bit to get back on treatment. Mo agreed. At our next appointment, we were told that the tumors in Jim’s lungs were still growing but, in true Mo style, he had one more thing to try, but this was it. If this treatment didn’t work, than he has exhausted all his resources.
Early in the morning of May 16th, Jim called out for me. I ran to him and he was struggling to breathe. We had an appointment later that morning in Iowa but I said to him, “Babe, I think we need to go to the hospital”. He agreed. The ER doctor told me the news that I knew, dreaded to hear, but knew I had to know. “He is dying” the doctor told me. I emailed Mo, I needed him to know. Oh, how I wish he could have been there, but we were too far away. I went in and told Jim “Babe, I think we are getting to end of our journey here”. We cried. I went to get our kids…family and friends gathered. By 10:15 that morning, my Jim was gone but I knew he was at peace.
The next morning I again emailed Mo. I thanked him for giving Jim three more years he may not have had. I told Mo to keep doing what he was doing…fighting for his patients in their battles against Sarcoma. And on our end, we will continue to keep doing what we have done for two years…raising much needed funds for Sarcoma Research through Drive Out Sarcoma.
I leave you all with this. Jim never complained, not about treatment, not about why he had cancer. He accepted his fate and trusted in Mo to help him. He also had a strong faith in God to help him through diagnosis, treatment and death. While the kids and I will miss Jim every day of our lives, we know he is at peace.
-Suzanne Burkhart